Originally published September 5, 2018.
This article on fevers is a segment of Raven’s teachings in her 2-part TCM Treatment of Pediatrics Class now available on-demand on the Mayway Education website.

Fevers are nature’s way of fighting off organisms that cause sickness by creating an environment that is inhospitable to pathogenic life forms. Fevers are also instrumental in developing and fine-tuning the immune system to deal with future illnesses. Even though seeing a child fever is hard to watch, it is foolish to silence it, because unless the system is challenged, the child will not develop strength and resistance. A fever arrives because the child is stressed or weakened or because there is a pathogen virulent enough to cause it. A high fever helps to fight infection by increasing white blood cells and it slows down the reproduction of the invading pathogen. When there is a fever, it is wise to help the child fight it on his own, by giving him appropriate foods, enough hydration, and herbal remedies. In today’s culture where both parents are working, it is common for children whose fevers have been suppressed by medications such as acetaminophen (Tylenol) or antibiotics to suddenly appear well, and as a result, the child is sent back to daycare or school. However, when the day is over, parents see that the medication given did not end the pathogenic experience, and the child remains ill. Most childhood fevers need to run their course and be followed by rest and replenishment. This is the key to building a strong immunity so essential for life.
One of the tasks for those of us working in a family practice is teaching parents the difference between fevers that can be dealt with at home and those that need to be seen by allopathic physicians. It is important for parents to realize that it is not necessary to consult physicians for each and every fever, and it is, more often than not, unnecessary. Most childhood fevers are viral in nature and are often seen with colds and flus. It is important to remind parents that fevers often appear after immunizations.
A good rule of thumb for any fevering child is to keep them away from drafts and air conditioning while ill and to keep them at home for two to three days after the fever has disappeared. This is important because it is easy to be attacked by wind or cold during a fever and in the days following one. During those few days spent at home and before returning to school or daycare, the child can rest and replenish.
Learning How To Assess a Fever That Needs Allopathic Care
Generally, when there is a fever in a newborn, seek an allopathic diagnosis. For children beyond neonatal life, a fever that does not resolve after 48 hours, despite careful attention, could be bacterial in nature and the child may be unable to easily resolve it on his own. It is at this time that allopathic assistance may be called upon.
When we evaluate or suspect problems such as kidney infections, pneumonia, appendicitis and meningitis, we need to refer these out for further assessment and treatment. When a child is crying out in pain, struggling to breathe, unconscious, or unresponsive, it’s time to call the doctor. Some of the conditions that can cause these symptoms are meningitis, appendicitis, kidney infection, and pneumonia. For these illnesses, allopathic treatment is preferred over TCM treatment. Even if you have needle patterns and/or herbal formulas for these conditions, it is inappropriate to use them when we have quick and effective allopathic treatments available. The ancient ways of using TCM methods are powerful, but they are also slow and during this time permanent damage to an organ can happen.
To check for meningitis, press the spine at the level of the neck or ask the child to put their chin on their chest. If either of these maneuvers produces what appears to be severe pain, consult a physician. Meningitis also produces severe headache and irritability. However, in babies under three months old there are often no symptoms of neck tenderness, and pain may or may not be present.

To check for appendicitis, you can do a rebound tenderness palpation in the lower portion of the abdomen and if the pain is severe, look for other signs to confirm your diagnosis. Typical signs of appendicitis include constipation, a red tongue with thick fur, a rapid pulse, and often an inability to walk upright or to lift one leg off a bed holding it straight, while in the lying down position. There will be pain along the Large Intestine meridians and also pain in the Stomach channel at Zhu San Li/St 36, and Lan Wei Xue/St 37.
To check for kidney infection, look for back pain - typically unilateral, pain along one side at the level of umbilicus, groin pain, stomach pain, vomiting, headache, and tenderness when percussing or tapping the kidney along the UB meridian. Wei Zhong/UB 40 and Ying Ling Guan/Sp 9 and San Yin Jiao/Sp 6 will be tender with palpation. Chills will likely accompany the fever and there will be frequent urinary output that may or may not be accompanied by pain.
To check for pneumonia look for dyspnea, coughing, sweating, a lack of appetite, a fever that could range from low to high, afternoon or middle of the night sweating, coughs that worsen at night, mucous, and weakness. Learn to auscultate lungs and listen for phlegm, rapid breath and heart rates, wheezing, and poor oxygen exchange. Breath sounds should be full, clear, and heard throughout the largeness of the lungs. Using a stethoscope, listen to the upper, middle, and lower areas of the lungs. It is easier to hear sounds when listening posteriorly, but if the child will not allow access to his back, listening to the anterior sounds also works.
Areas to listen to are: posteriorly UB 11 or UB 42 (under clavicles for upper back), UB 14 or UB 43 (between the scapula) for middle back, and UB 17-18 (at lower border of the scapula) for lower back. If listening anteriorly, listen at K 26 for upper lungs, K 22 for middle lung and GB 24 area for lower lungs. If sounds are small, shallow, weak, with barely a sound of air whooshing in and out or an absence of sound, the exchange is poor and the child needs help. If you hear wheezing, rumbling, crackling, bubbling, or sounds like snoring, this indicates lung disease or infection. To begin listening to lung sounds, each time you see a child, spend 30 seconds or so listening. If sounds are clear and full you can continue on with your treatment. If sounds are not clear and full, listen carefully, find the spots that are the most telling of the disease, and go from there. Newborns or infants may not actually have altered breath sounds that show infection, but may vomit, have a fever or cough, and appear restless, listless, or without Qi.
For the child’s safety, and your own, each of these conditions needs to be taken to an allopathic physician for further evaluation.
Learning To Assess A Fever
Having been a midwife and seeing women at birth centers who also had their kids with them, there was plenty of opportunity to evaluate kids who were coughing, acting out, crying, etc. During those birth center days, I learned a quick method of assessing the child in question, and it didn’t require a thermometer, an otoscope, or any other tool. If there is a thermometer, it can be used for confirmation of findings, and in that situation, is a great teaching tool.

When assessing a fever, check the temperature of the skin, especially the axilla. You can also feel the head, especially at Tai Yang, and this can be done with the back of your hand, which has greater sensitivity to temperature changes than your palm. If a child resists the thermometer or the parent wants a quick way to assess a fever without resorting to a thermometer each and every time she wonders if there is a fever or not, you can teach the mother to feel for heat in the child’s axilla or to use her cheek against Tai Yang, which was the way I was taught by my grandmother to take a temperature. If these areas are especially hot, you will know right away that there is a fever, and taking a temperature with a thermometer will tell you exactly how high it is. A normal temperature is 98.6 degrees Fahrenheit if taken orally and one degree less if taken axillary. It’s important to wait ten minutes if the child has just ingested something hot or cold, or the reading could be inaccurate. When the fever is high, respirations and heart rates are elevated.
I find a good method for measuring the heat/fever is by listening to the heart and counting the beats within a specific amount of time, such as 30 or 60 seconds. When the heart is beating very fast, you can be sure the temperature is over 101. It’s important to know the normal range of heart rates in babies, toddlers, and children, as they are very fast at the start of life and decrease by increments as growth and years pass. Newborn babies have very rapid heart rates, with the most normal rate being approximately between 130 and 145 beats per minute. (The normal range for a newborn is 120-160.) Learn how to count this rate. You will need a watch with a second hand on it. As children age, their heart rate decreases, so that by age one a normal heart rate might be down to 120 per minute, and by two years old it may be down to 108. Pay attention to the rate of a heart-beat at each visit, because children vary in rates, and you will want a baseline for each individual child.
Yang children will have faster heart rates, and Yin children will have slower ones. So, if you get a child whose heartbeat is 130 at a year, and is Yang, loud, strong, and resilient, with no symptom or complaint, then you will not think this is too fast or a problem. If you have never seen the child before, then take this rate, note it, and compare it with the next visit and the one after that. Taking a rate at each and every visit and noting it in your chart helps you to get an individual baseline as well as more accurately diagnose a problem. So, if we return to the child whose heartbeats are 130 a minute and is one year old with no complaints or symptoms, and you take the temperature just to see if the reading is within normal limits, and it is, this will then confirm that this heart rate is normal for this child. However, another child who runs cold, is thin with a poor appetite and clings to the mother may have a much slower heart rate normally, and if he appears with a 130 heart rate at one year, with symptoms and complaints, and heat is palpated at the temple and/or the axilla, you can bet there is a fever. Individual heart rates must be factored into your diagnosis. When one diagnoses a fever through hands and ears (auscultation of heart-rate), a thermometer is used to confirm findings and diagnosis.
Eventually, when you’ve seen enough children, you will no longer need the thermometer, unless you want to confirm your findings. The skill of touching and palpating will season a practitioner to assess fevers without needing tools external to one’s five senses. This then enables you to assess a fever while being anywhere at any time.
How To Assess A Fever Without Using A Stethoscope
Often a fevering child does not want his temperature taken or his heart listened to. If this is the case, and you are a beginner, then face the child’s back so you are out of vision, put the stethoscope on the child’s chest or on their back behind the heart, and ask the parent to distract him while you count. Work quickly and work so that you get at least three or four five-second intervals to count, and then multiply by 12, since there are 12 five second intervals each minute. For instance, if you count three different five-second intervals at 9 beats each, multiplying 12 times 9 equals 108. If you count approximately 30 beats every 15 seconds and multiply by four, you will get 120. If you count 18 beats in a ten second interval, you would multiply by six and this will be 108 per minute. For those of you who are lucky enough to have a little one in your family, you can begin to learn how to take a heart rate at home so that you can get quick with this skill and make a fast assessment of heart-rate. One wants to work quickly with children because they are often in constant motion, or they will resist a new person touching them, especially if they are sick and not familiar with you or your space.
When you get a baby under six months old who is hot, red faced, and whose heart is beating around 170 beats a minute, you can be sure there is a temperature, and it is usually at least 102 degrees, or higher, closer to 103 or 104.
It is important to know that if using medication, acetaminophen (Tylenol) is hard on the liver, so ibuprofen (Motrin) is a better choice. However, essential oils can also be effective. Dilutions in carrier oils of peppermint, wintergreen, copaiba or eucalyptus oil can be rubbed on the skin along the associated organ Shu points or a few drops can be added to a diffuser and taken in via the lungs. These are common oils known to reduce fevers.
High Fevers
Remember that children tend to fever high, and temperatures of 103 and 104 degrees are not unusual. Children who have strong Qi consistently fever high. Children with temperatures of 104 degrees or higher, for over 2 ½ days, who are not able to sleep, eat, or drink, and are not responding to your needles or herbal formulas, need to be sent to an allopathic physician for evaluation. Most viral conditions resolve the fever or have it decrease by 48 hours, but bacterial infections will linger and not resolve.

However, once you get to know a child and see their pattern for fevers, or for children who consistently fever high with viral conditions, keep this in mind and do not panic. Some children just run very high fevers for simple problems such as teething or viral conditions, and parents need to understand this while they keep the fever from getting too high by using techniques and herbs designed to do that.
Children who fever high should have a cloth that is several degrees lower than their body at their neck and their head or temples. Initially they might resist this, because the cloth will feel cold and uncomfortable to them, but within seconds the cloth will warm. Always begin this application slowly so that the child is not shocked by the change in temperature. Once you begin this, keep the cloth cool by dipping into tepid water, and keep applying. This will temporarily reduce the fever and provide safety to the brain. However, this should not be done day after day without medical supervision. I have known some parents whose children consistently fevered high at 105 degrees for viral conditions, after immunizations, or teething, who would use an ice pack wrapped in a towel and applied to the vertex of the head or the nape of the neck during the height of the fever.
Deficient children are less likely to have high fevers but they can be as sick or sicker than a child with a high fever and you will know this through their behavior. If they are fevering, not drinking or nursing, and are lethargic or crying weakly for more than 48 hours, they should be seen and evaluated by an allopathic physician. Most children have at least several high fevers in their lifetimes, and do well through the course of the fevers, but you must make sure that the child is not dehydrated or too sick to fight the fever without medical help. Always teach the parents to hydrate a child or baby when there is a fever.
Beginning practitioners might feel unsure of evaluating a baby who is fevering high. If this is the case, refer the baby or child to a more seasoned practitioner, pediatrician, or general practitioner whom you know and trust. Teamwork is educational and it is always better to be safe than sorry. Once I saw a new patient who was a 12-month-old baby fevering at 105.5 and had been for three days. With the mother’s permission, I bled the baby and gave her half an ounce of an herbal formula (Xiao Chai Hu Tong) and then sent the mother and the baby to a seasoned GP nearby. When the mother and child arrived the doctor evaluated the baby, put the little one in a sink with tepid water, and said the condition was viral, as there were no signs of deep conditions such as meningitis, appendicitis, etc. Also, by the time the baby arrived at the office, the fever had broken due to the bleeding and herbs, but the doctor said even if the fever had remained 105.5, he would have done the same thing and then watched and waited. This ability to evaluate and rule out conditions that need allopathic treatment or medication takes time to cultivate, so be gentle with yourself if you are a beginner. We all need to learn, and practice gives us the experience we need to become seasoned properly in order to evaluate when our medicine is appropriate and enough for any given condition.
Seizures
There is always the chance that a fevering child will have a seizure. These are called febrile seizures and occur when the temperature is over 102, especially when a fever rises suddenly. The word “sudden” shows that Wind, the leader of 100 diseases, has taken place, so the best treatment is to prevent a sudden rise of temperature. This is done by sponging the child with tepid water or applying a cool cloth to the head, temples, or neck, and keeping the child in a cool environment and clothing.

Febrile seizures can have symptoms of jerking or twitching for mere seconds or convulsing from 1-2 minutes and on rare occasions up to 10 minutes. Long seizures can have a loss of urine or bowels, loss of consciousness, or eyes rolling back into the head. If this occurs, after the seizure bathe the child in water three to four degrees less than her temperature to bring the fever down temporarily. If you see this or talk to parents who are seeing a seizure, advise the parents to lay the child on the floor away from objects and furniture and on her side. This will prevent the child from falling off a bed or hitting herself with sharp objects as well as preventing her from aspirating any food or fluid in her mouth while seizing. What is important here is that the parents do not panic, because what the child needs is their calm and reassurance. There are some children who consistently seize with fevers and parents learn how to stay grounded and attentive during them without running to a hospital each time it occurs, as emergency rooms are forced to do a lumbar puncture with children who are fevering high and convulsing.
After a seizure, bathe the child in water three to four degrees less than her temperature to bring the fever down temporarily, or give the child ibuprofen (Motrin). However, if seizures continue during one illness, the child needs to be seen by an allopathic physician for evaluation. Most seizures occur to babies between 12 and 18 months, although they can occur from 6 months to 5 years of age.
Clothing
Be sure to instruct the parents that their child only wear cotton during fevers. Cotton breathes whereas synthetic cloth holds in the heat and the toxin, raising the temperature further. When I lived in British Columbia on Vancouver Island, I knew of an 18-month-old child whose parents I midwifed. The child had bronchitis and was fevering. It was the dead of winter where it was dark by 4 PM, and the only heat in the house was wood heat, which was in the main room. The bedroom was in a different corner of the house and was always freezing cold. That night was snowing and you could see your breath inside the house.During the night the parents dressed their child in a synthetic onesie, and put a little cap on her head. They had a down comforter on their bed, but because it had been so cold they had a few extra blankets, and then they put the child in between them for the night, thinking that they were doing the right thing. When they awoke in the morning their baby was dead. I tell you this because the proper dressing of a child who is fevering is essential to understand, and putting them in a relatively cool environment is also of the utmost importance.
You cannot gauge what clothing a fevering child should wear based upon what you are wearing. In this instance, gauge their clothing by their heat. Also, clothes with the colors red, orange, and bright yellow are not good for fevering children. Colors should be cool, like mint green, sky blue, or white. When a child is fevering, do not cover the head and do not cover in multiple blankets. To assess if a child is cold or not while fevering, insert a hand under the clothing and onto the thigh or shoulder. If they are warm, despite a cold nose or cold hands, the child is warm. Also, remember to not put a fevering child in a draft or in an air-conditioned room.
Foods
While a child is fevering their appetite is normally gone. However, you must hydrate them. For nursing babies and children this is not difficult, as they tend to want to be at the breast for nearly continual feeding.For children who are not nursing, this is most easily done with lemon water, watered down juices, or cooling teas such as catnip, elderberry, chrysanthemum and honeysuckle. Even adding a teaspoon of maple syrup to a cup of hot water is acceptable. Cooling foods such as fruit popsicles, clear liquids, broths, or melons—specifically honeydew, watermelon, and cantaloupe are also good. Bananas, grapefruit and mulberries are cold, and blueberries, lemon, pear, persimmon, and strawberries are cooling. If they can sip a broth or eat gruel, barley is a cold grain, and brown rice and pearl barley are cooling ones, and a touch of maple syrup can be added for compliance.
Most children will refuse food when fevering high, but if you have little bites of different types of melons available and presented like bite size little balls, the child may accept them, one bite at a time. Always keep a few drinks by the bedside of a fevering child. If the child is too old for a bottle, then have a bendable straw. Avoid foods that bind the bowels such as rice or wheat. Remember that bowel movements are a way of moving the heat out.

A few drops of wintergreen or peppermint oil in a carrier oil can be rubbed on the Shu points along the Urinary Bladder meridian, the soles and palms of the feet and hands, or a drop or two of the essential oil can be added to a drink. A few drops of eucalyptus or nutmeg oil can be added to ¼ cup of water.
After the fever breaks, give foods that are easy to digest, such as the congee suggested above. If the child craves a particular food, follow that craving. Remember to continue to hydrate. A healthy ginger ale could be helpful because it aids digestion and is seen as a prize sort of drink, which helps with compliance. Pears quartered, covered with water and cooked are good to reduce phlegm in the lungs and are often readily accepted because they are sweet and delicious. Diluted amazake made from rice koji is good after a fever because it is nourishing and easy to digest. If there is phlegm, Lo Han Guo cubes are good because they are sweet, will nourish the lungs, and hydrate once made into a tea. Don’t forget “Recharge” for older children, which is a drink that balances electrolytes and is always helpful after a fever.
The Element of Water
Water is a method that is almost always available. As already stated, a tepid bath 3-4 degrees cooler than the child is helpful in temporarily reducing a fever. Again, what is important here is that the water should not be too cool or the child will cry from the shock of it. A brew of mint or lavender flowers, or some drops of Wintergreen or Peppermint oil can be added as well as oils already mentioned, as these will assist the water in cooling the heat. If you have lavender flowers, make a brew, dip the cloth into it, and while in the bath, sponge the head with this.

Another method of bringing down the fever that I learned from my beloved teacher Dr. Miriam Lee is a ginger infusion footbath. To do this, grate or slice fresh ginger and put into a pot big enough to immerse the child’s feet into. Bring the water and ginger to a boil for twenty minutes so the water is infused with the ginger, and when it has cooled down some, bring it to the child and immerse the feet into it. The water should still be relatively hot, but not hot enough for the child to resist it. I have encouraged the parent to also put toys and maybe even flowers into the pot, which makes the footbath more interesting. Keep the feet in this for as long as the child will let you, and if the water cools down too much but the child is still enjoying it, just add more hot water. Snuggle the child at this time, give him a foot rub, read a story, or let him splash in the water. Just try to keep the feet in the water for enough time that the feet turn pink and are toasty warm when they are removed. This method pulls the heat out of the head descending it into the feet and gives comfort by reducing headache, heat in the Upper Jiao, or just cooling the head to reduce the fever. You can repeat this footbath several times during the day. Besides being physically therapeutic, this is a very healing thing to do energetically. If your child is unable to participate in this bath, then put some sliced ginger between two pairs of socks and it will work in a similar manner.
Bowels
If the child is only moderately fevering 99, 100, 101, or 102 degrees, and has not moved the bowels, encourage laxative foods or laxatives. Since the bowels retain the heat and toxin, when there is movement, the fever can automatically diminish or sometimes even disappear. Prune juice is good for this, or stewed apricots and prunes. Both the fruit and the juice are helpful in lubricating the bowels and since they are sweet, there is mostly compliance. If a dozen of each fruit are stewed, then continue to feed this to the child until the pot has been emptied as well as the bowels. Again, do not feed foods that bind the bowels such as rice, bread, pastas, pizza, and peanut butter, as they slow down elimination.
You can also promote bowel movements by running your hand in a quick stroke downward on the child’s sacrum (Tuina) and this can be repeated 50 to 100 times within a minute or two. For an infant or toddler, this is most easily done when one parent holds the child in the burping position, and the other parent does the downward strokes on the bum. This directs the Qi downward and awakens the bowels. For an older child, lying on the belly is another good position for this Tuina technique. You can also put pressure on Gv 1/Chang Qiang, or even press or tickle the anus, as this often awakens the bowels. For very stubborn cases, you can glove up and with your pinkie finger stimulate the sigmoid colon for evacuation. Once the bowels move, the child should be peppier and the fever should reduce.

If you have tried all the above suggestions and the child still has not moved his bowels in 24 hours or more and has a high fever, consider an enema. If the child is a newborn or an infant, the enema dose is 1 or 2 droppers (from a one to two ounce dropper bottle) of warm oil. For a child three to six months old, more will be needed. For children older than that, you can instruct the parents to use a bulb syringe, the type used at birth to suction out the mucous from the mouth and throat. The syringe is filled with warm water, catnip tea, or water mixed with oil (such as organic cooking oil), and the contents should be warm and not below room temperature. Vaseline or oil rubbed onto the child’s anus so the insertion will be easy is helpful. Instruct the parents to slowly insert the bulb and then also slowly and steadily release the contents of the syringe till it is empty. Totally remove the bulb syringe from the colon while continuing the compression on the bulb syringe. The child should move the bowels quickly after this enema, so it’s important for the child to be near a toilet or on a large diaper when the enema is given. If the fluids are expelled but the bowels do not move within one to two hours, repeat this procedure at least one more time and expect a bowel movement within the next hour. If one cannot get the bowels to move and the parents feel that the colon is full and the fever remains, it is not a good sign and would be a good reason to see an allopathic physician.
There are also instances when the child is fevering high, the enema is given, and there is no result of a bowel movement nor does a drop of water come out. When this occurs, the child is so dehydrated that the bowels take up the fluid, which actually hydrates the child. For children who are fevering high and refuse to drink, this has worked for hydration. Repeat this procedure until the bowels no longer take up the fluid. If this level of dehydration persists, the child must be seen by a medical doctor or taken to an ER.
Caution: You will not do or advise an enema for a child whom you suspect has a bowel infection such as appendicitis or a bowel obstruction. For these cases you refer the child to an allopathic physician.
Since pediatric fevers are part of any family practice, it is important to understand the complexities of them, learn to assess them with the tools nature gave you, and know when to refer to an allopathic doctor. But it is equally important to teach these skills in assessment, observation, and good common sense to parents, who are after all, their child’s first pediatrician.
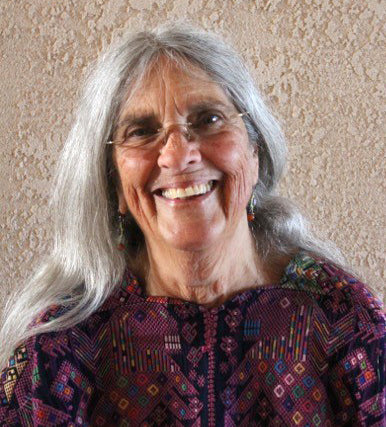
About the Author

Raven Lang, L.Ac., O.M.D. is a popular and well-respected instructor, having specialized in TCM treatment of women and pediatric patients for over 30 years. She has been teaching about natural childbirth for nearly 50 years and wrote the first book on home birth as well as opening the first birth center in North America in 1972. She worked as a midwife, founding the first non-medical midwifery school and in 1982 began to study TCM. a year later was blessed with a three-year apprenticeship with Dr. Miriam Lee, a nurse midwife from China and one of the first licensed acupuncturists in California. Raven incorporates her knowledge of midwifery, mothering, and traditional medicine (both American and Asian) in her work and brings a wealth of experience to those she serves. Now retired, Raven practiced TCM in Santa Cruz, California for over 30 years.