Stabilizing Shen and Hun: Insomnia
Reprinted from Clinical Handbook of Internal Medicine (2nd Ed.) by William Maclean with permission of Eastland Press. Buy the book
Insomnia (bù mèi 不寐, shī mián 失眠) is difficulty sleeping. Insomnia includes inability to sleep, difficulty falling asleep, frequent waking, restlessness at night, a disordered sleep cycle and dream disturbed sleep.
Most adults sleep 7 to 8 hours per night, although the timing, duration and internal structure of sleep varies considerably among apparently healthy individuals, and as a function of age. Assessment of a patient complaining of insomnia should distinguish true insomnia from transitory insomnia due to external or temporary changes.
Ambient noise, weather changes, inappropriate bedroom temperatures, consumption of coffee or other stimulants prior to bedtime, eating late, screen time, recent emotional upsets, vigorous exercise and the disordered biorhythms of shift workers may all cause a person to sleep poorly. Once these factors are removed and sleep usually returns to normal, the sleep disturbance cannot be considered true insomnia. Similarly, sleep disturbance due to pain, itching, asthma and breathing disorders should not be diagnosed as insomnia.
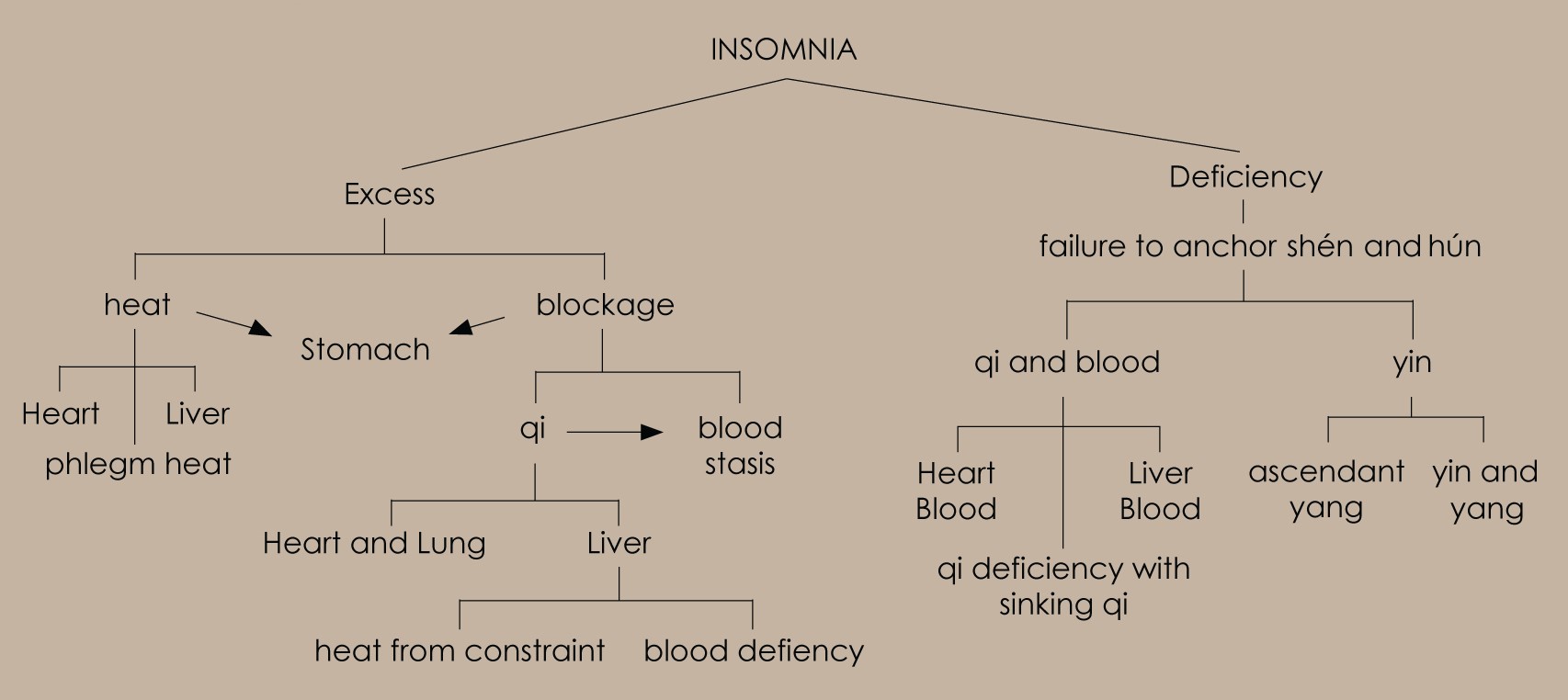
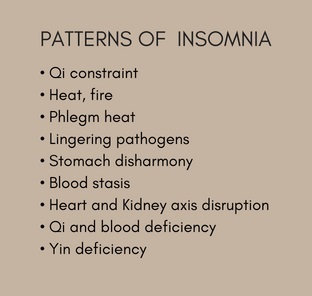
In Chinese medicine, insomnia is primarily associated with instability or agitation of the anima, the shén and hún. This occurs because:
- The shén and hún are not adequately anchored and secured due to insufficiency of blood or yin.
- Over stimulation and agitation by heat prevent the shén and hún from settling quietly when the time comes for sleep.
- The shén and hún are constrained and agitated by qi and blood stasis or phlegm.
- Yin and yang are out of balance, and an excess of ‘yangness’ interferes with the yin resting phase of the daily cycle.
ETIOLOGY
External pathogens
Many acute external pathogens will cause temporary sleep disturbance, which is corrected when the acute illness resolves. More persistent insomnia can occur in the aftermath of a febrile illness that damages yin, or an acute external pathogenic invasion that is poorly managed. In the first case, yin damage leads to heat from the deficiency with consequent shén disturbance. In the second, acute infections treated inappropriately with antibiotics, bitter cold or purgative herbs can lead to a lingering pathogen. Once a lingering pathogen is in situ, the heat generated by its presence easily disturbs the shén. Lingering pathogens are a common source of insomnia, potentially persisting weeks or months after the initial illness.
Emotional factors
Emotional factors are an important contributor to sleep disturbances. The most common involve constraint of qi flow through the Liver system, disruption of the Heart Kidney axis, and generation of Heart fire.The Liver system is constrained, with the Liver’s regulating and distribution of qi impaired by internalized and repressed emotion, in particular frustration, anger and resentment. Disruption to the internal rhythms of the sleep wake cycle by shift work or activities that run counter to the yin phase of the daily cycle also contribute to qi constraint. When Liver qi is constrained, it disrupts the generative cycle of the five phases resulting in poor support for the Heart. Constrained Liver qi also disturbs and irritates the hún. Persistent qi constraint leads to blood stasis and can generate heat or fire. Any heat in the system agitates the shén, damages yin and congeals blood. The more heat, the more damage and agitation. Liver fire is more likely in those with a yang or hot constitution, and those ingesting a heating diet, stimulant drugs and alcohol.
In the young, the Heart Kidney axis is robust, so disruption of the axis requires a major shock or emotional trauma. This may be something in the order of the death of a loved one, a motor vehicle accident, the result of experiences in a war or some environmental catastrophe. In older people, with some shào yīn weakness from age, overwork or other factors, the trigger event for disruption of the Heart Kidney axis can be more trivial.
Chronic anxiety, worry, sadness and grief retard the movement of Heart and Lung qi. The resulting accumulation of qi creates a focus of pressure in the chest, which can generate heat or fire. Heart fire may also develop if fire is transmitted from the Liver to the Heart. Heart fire is more likely to occur in those with some pre–existing heat, whether from diet or constitutional factors. Persistent heat in the Heart damages yin.
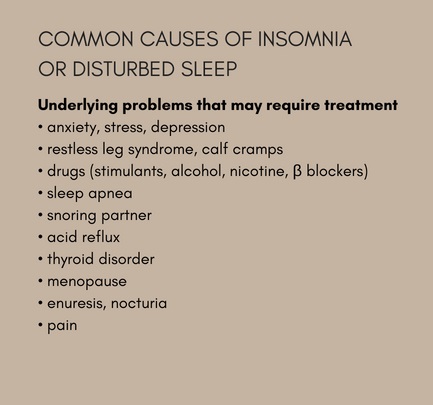
Diet, medications and drugs
Two aspects of diet contribute to insomnia; those that create excess of some kind (heat, phlegm heat, food stagnation) and those that lead to deficiency of qi and blood. Factors that lead to an excess pattern include overeating, eating late at night, and consuming excessive amounts of heating or phlegm damp forming foods and alcohol. Those leading to qi and blood deficiency are those that weaken the Spleen and Stomach; irregular dietary habits, overconsumption of cold raw foods, insufficient food intake in general, or inadequate amounts of building blocks required to manufacture qi and blood like protein, in particular.Long-term stimulant drug use, including substances such as cocaine, speed, methamphetamine and caffeine in large doses, seriously plunder Heart yin and essence, leading to chronic health and sleep problems. Many people with transitory insomnia, or sleep problems associated with emotional states start using tranquilizing and hypnotic medications, which may be habit forming, even after relatively short periods of time. When withdrawn, some of these medications lead to reflex insomnia and a cycle of dependency.
Exhaustion, overwork, constitution
Overwork, physical and mental exhaustion can weaken the Spleen and Kidney and impair generation of qi and blood. Qi and blood can be depleted if more is used in activity than can be replaced by the Spleen; this can sometimes be seen in athletes with high intensity training schedules, or in the context of a prolonged or severe illness. The primary weakness in such cases is of the Spleen, which is unable to generate enough blood to nourish the Heart and anchor the shén. Spleen and Heart deficiency can also be more acute, following a postpartum hemorrhage, difficult pregnancy or labour. Spleen and Heart deficiency is quite common in women who return to work too soon following pregnancy, without fully recovering their qi and blood. It also occurs in those who breastfeed for lengthy periods of time while expending energy working or looking after demanding families. 
Kidney and Liver yin are consumed by overwork, excessive reproductive activity, insufficient rest, ageing, stimulant drug use and any prolonged heat in the system. Kidney weakness fails to support the Heart, the Heart and Kidney axis disengages and the controlling cycle disrupted – Kidney water no longer balances and restrains Heart fire; fire flares uncontrolled and the shén disturbed.
A tendency to sleep problems and emotional fragility can be lifelong. Technically known as Heart and Gallbladder qi deficiency, it describes a personality type that can be congenital or acquired. When congenital, it is inherited from weak or elderly parents or due to a significant shock that damaged the developing fetal shén during the mother’s pregnancy. When acquired, it can be seen in individuals raised
in an abusive or fearful environment, or in adults or children who experience a violent or extreme shock or fright. It can occasionally follow other debilitating illnesses that plunder qi.
The involvement of the Gallbladder here refers to the timidity and ‘lack of gall’ (that is, fearfulness) that characterizes these patients. In the Chinese language, as in English, there is an implicit understanding of the relationship between the Gallbladder and courage, indeed to be bold and courageous is to have a ‘big Gallbladder’ (dà dǎn 大胆), whereas to be timid, nervous or cowardly is to have a small Gallbladder (dǎn xiao 胆小).
Habit formation; resetting circadian rhythm
Persistent sleep disturbance can reset the sleep cycle. This is seen in shift workers, frequent flyers and new parents with poor sleeping babies. The sleep disturbance interferes with the sleep cycle in such a way that even when the source of the disturbance has passed, i.e. the baby sleeps through the night, shift changes, etc., sleep remains disturbed. In Chinese medical terms it is usually the Liver that has been upset, with qi constraint and its various consequences the result. This type of insomnia requires a retraining approach to sleep, with a strict bedtime routine and sleep hygiene, in addition to specific therapeutic intervention. Acupuncture is especially helpful in this type of insomnia.Trauma
Insomnia following an external trauma, physical or head injury is usually due to blood stasis. On occasion an extreme emotional shock or physical trauma can disconnect the Heart and Kidney axis, leading to a yin deficient or qi deficient pattern.TREATMENT
Acupuncture and herbs produce reliable results in many patterns of insomnia, and are of great assistance as patients gradually wean themselves of tranquilizers and sedatives. 
Sleep hygiene is important. Adjuvant therapy is useful in most types of insomnia, particularly relaxation or meditation to calm the mind.
The most important distinction is between excess and deficient types, with excess patterns tending to be more difficult to treat than the deficient types as there are often complicating lifestyle factors beyond the practitioners control – unhappiness or stress at home or at work, deleterious behavior patterns and habitual mental emotional responses that have to be dealt with for a satisfactory result. Conversely, deficient patterns generally respond well to treatment, although this needs to be combined with an appropriate nourishing diet.
Not infrequently, cases of insomnia are seen in which no clear pattern can be discerned. These are typically associated with resetting of the circadian rhythm, occasionally atypical blood stasis (that is, blood stasis with few if any of the classic systemic features).
Management of internal cycles is a function of the Liver organ system, therefore treatment focuses on regulating the Liver to restore its management of cyclical change. Acupuncture is the treatment of choice and the protocol noted in the Liver qi constraint section can be followed.
When all else fails, the default strategy is to regulate and invigorate blood, which sometimes produces surprisingly satisfactory results.