Fainting and Funny Turns: Part 2
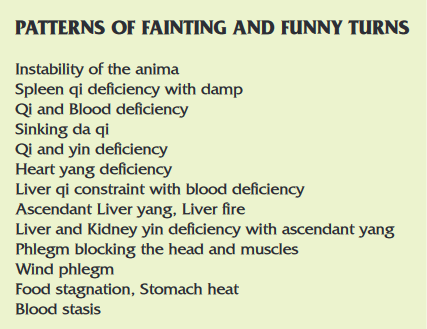
Patterns of Fainting and Funny Turns
Instability of the Anima
The anima referred to here are the shen, hun, po, yi and zhi. The pathology derives from their lack of grounding, without which they are easily destabilized and scattered by external events. The traditional description of this disorder is Heart and Gallbladder qi deficiency (xīn dăn qì xū 心胆气虚). The Heart and Gallblader (and by convention the shen and hun) are designated as the primary site of the pathology, and it describes a patient with a constitutional or acquired tendency to nervousness and anxiety. The Gallbladder qi deficiency is a reference to the timidity and “lack of gall” (that is, fearfulness) which characterizes people with this pattern. In the Chinese language (as in English) there is an implicit understanding of the relationship between the Gallbladder and courage, indeed to be bold and courageous is to have a “big Gallbladder” (dà dăn 大胆). In practice, any or all the anima may be affected, and the manifestations vary accordingly.
Instability of the anima is a state in which the patient is hypersensitive to external influences, perceived threats and sudden change, and has insufficient protection or boundary. Their response to an anticipated or current event is out of proportion, and because the anima are already tenuously grounded, trivial events are enough to unhinge them sufficiently to disturb consciousness, resulting in sudden fainting.
Clinical features
- Sudden fainting in response to social or psychological stress of some type, preceded by flushing, hyperventilation, palpitations and sweating. There may be tunnel vision, loss of bladder control, sleep disturbances and disturbing nightmares or agoraphobia.
- Long term tendency to nervousness and timidity, fearfulness and anxiety, poor self image and emotional instability.
- T: unremarkable or variable depending on complicating pathology
- P: generally thready, but may be variable, depending on complicating pathology
Treatment principle
- Stabilize the shen and anima
- Strengthen the Heart & Kidney (as foundation of other anima)
Variation
With a sensation of energy rushing up to the head
Fainting may be preceded by a sensation of energy rushing upwards from the epigastrium or abdomen. This sensation is described as ‘running piglet qi’ (ben tun qi 奔豚气), and is precipitated by instability of the Heart and Kidneys. A sudden fright or shock, or even a sudden loud noise, can be sufficient to disrupt Heart Kidney communication, leading to acute qi counterflow. The treatment is to reconnect the Heart and Kidneys, lead the ascendant qi down and support qi blood.
Key to symbols following acupuncture points:
- absence of a symbol denotes an even method
- + apply a supplementing method
- - apply a reducing method
- ∆ use moxa; stick, warm needle, rice grain, moxa box etc.
- ↓ bleed with a surgical lancet
Acupuncture (select from)
- 19 (houding), Du.20 (baihui), Du.24 (shenting), Yin Tang (M-HN-3); these points calm the shen
- 14 (juque) alarm point of the Heart, calms the Heart and shen
- 15 (xinshu +) transport point of the Heart, supplements Heart qi, calms the Heart and shen
- 7 (shenmen +) source point of the Heart, calms the shen, regulates and supplements Heart qi
- 23 (shenshu +), Bl.52 (zhishi +); these points supplement the Kidneys and stabilize the zhi.
- with anxiety and aversion to social interaction, add Lu.3 (tianfu), Bl.13 (feishu ∆) and Bl.42 (pohu)
- with fearfulness and loss of bladder control, add Kid. 4 (dazhong) and Ren. 4 (guanyuan ∆)
- with disturbing dreams, add Bl. 47 (hunmen), Bl.18 (ganshu) and Liv.8 (ququan)
- with tightness in the chest and palpitations, add PC.6 (neiguan)
- Ear points: heart, shenmen, sympathetic
Clinical notes
Fainting of this type may be associated with personality type, autonomic nervous system dysfunction, hyperventilation, conversion reactions, hysteria or vasovagal syncope. The prognosis for fainting from an unstable animus is variable. When constitutional, the prognosis is poorer than from when the condition is acquired later in life. However, some patients do surprisingly well, and become much more confident and self-assured. Regardless of etiology, treatment needs to be consistent and prolonged. Regular, long term acupuncture seems to be the most effective intervention.
Spleen Qi Deficiency
The Spleen is responsible for the harvesting and maintenance of adequate levels of qi and blood. When the Spleen is weak and qi levels low, even a slight increase in usage of qi can lead to a failure of Spleen qi’s ascent and inadequate qi getting to the head.
Clinical features
- Sudden light-headedness, tunnel vision, feeling of not being present or fainting, usually in response to hunger or following a period of increased activity. Episodes are more likely to occur in the afternoon, and are accompanied by pallor, sweating, palpitations and hunger. Recovery may be gradual with the patient quite groggy for a while.
- In between episodes
- fatigue and tiredness that are better for rest and worse at end of day
- appetite that varies between indifference to food and gnawing hunger; sweet cravings, abdominal distension, early satiety
- loose stools
- muscles easily fatigued and tired; muscle weakness, poor muscle tone
- spontaneous sweating
- T: pale, swollen and scalloped and a thin white coat
- P: weak, thread
Variation
Spleen qi deficiency with damp
Spleen qi deficiency is often complicated by damp. The damp settles like a mist over the mind, so foggy head and difficulty in concentration are more pronounced, sometimes to the point of disorientation, or a momentary lapse of consciousness (‘spacing out’) in the middle of a conversation. The lack of energy resulting from qi deficiency is compounded by a sense of heaviness. The patient will want to lie down and sleep, especially after eating and more so in the mid afternoon, but will wake feeling worse. The tongue is pale and swollen with a thick, greasy, white coat. The treatment is to strengthen the Lungs and spleen, supplement qi and transform damp.
Acupuncture (select from)
- 12 (zhongwan +∆) alarm point of the Stomach, strengthens the Spleen and Stomach and supplements qi
- 36 (zuzanli +∆) sea point of the Stomach, strengthens the Spleen and Stomach and supplements qi
- 3 (taibai), St.40 (fenglong); these points strengthen the Spleen and transform damp and phlegm.
- 20 (baihui ∆) clears the head and elevates qi
- 20 (pishu +∆), Bl.21 (weishu +∆) transport points of the Spleen and Stomach, warm and strengthen middle burner qi
- with foggy head, add Bl.62 (shenmai)
- with edema, add Sp.9 (yinlingquan -) and Sp.6 (sanyinjiao)
- with abdominal pain, add Sp. 4 (gongsun)
- with diarrhea, add St.25 (tianshu)
- with abdominal distension, add St.25 (tianshu) and Sp.15 (daheng)
- Ear points: spleen, stomach, pancreas, zero point, endocrine, sympathetic
Clinical notes
Fainting and funny turns from Spleen qi deficiency are common and may be diagnosed as hypoglycemia or poor blood sugar regulation. Spleen qi deficiency, with or without damp is a common starting point for the development of type 2 diabetes mellitus. Spleen qi deficiency responds reliably to treatment. In most cases, the patient should expect some improvement within a few weeks, then restoration of digestive function and regulation of blood sugar levels over several months. Regulation of the diet is a crucial factor in long term maintenance. Moderate aerobic exercise, in particular walking, swimming, yoga, taijiquan and qigong are beneficial in strengthening the Spleen and Lungs.
Sinking Da Qi (Collapse of Heart and Lung Qi)
Sinking da qi is the result of failure of the Spleen, Heart and Lungs to maintain the integrity of qi against the pull of gravity. The da qi (which is synonymous with zong qi, the qi of the Heart and Lungs) is unable to maintain its position in the upper burner and slumps into the lower body, which impairs the function of the Heart and Lungs, and leads to compromised circulation of qi and blood. Qi and blood fail to reach the head and sudden fainting or scattered consciousness occur. Sinking da qi usually begins with transitory turns characterized by sweating, palpitations and light-headedness. As the qi becomes weaker and sinks for longer periods, fainting and drop attacks start to occur.
Da qi is weakened by factors that influence the Heart and Lungs. These include acute and chronic emotional stress (intense grief and sadness or loss, periods of extreme excitement or over-stimulation), physical exhaustion, excessive sweating, chronic diarrhea and excessive use of substances that disperse or direct qi downwards, such as medications for asthma.
Clinical features
- Sudden, transitory disturbance of consciousness, fainting or drop attacks. Episodes may be initiated by periods of increased or unaccustomed activity. Pallor, hyperventilation, sweating, confusion, disorientation or ‘feeling distant’ may precede an episode. There may be incontinence of urine, or feces. Recovery is gradual, with lingering fatigue and grogginess.
- breathlessness, rapid or laboured breathing, dyspnea, panting
- pale or ashen complexion, copious spontaneous sweating
- empty feeling in the chest; chest pain, palpitations, bradycardia
- lower abdominal fullness, distention and discomfort
- T: pale
- P: weak, thready, or imperceptible, especially in the distal (cun) position and clearly stronger in the (chi) position: or irregular and intermittent
Treatment principle
Supplement and raise sinking yang qi
Acupuncture (choose from)
- Du.20 (baihui +∆) lifts yang qi to the upper body
- Bl.13 (feishu +∆), Bl.15 (xinshu +∆); tranport points of the Lungs and Heart, these points supplement zong qi
- Du.14 (dazhui +∆) meeting point of the yang channels, an important point elevating yang qi to the upper body
- Ren.17 (shanzhong +), Ren.12 (zhongwan +), Ren.4 (guanyuan +∆); these points promote correct movement of qi in the triple burner and supplement qi
- Lu.9 (taiyuan +) source point of the Lungs, meeting point for the vessels, strengthens Lung qi and yin
- St.36 (zusanli +∆) sea point of the Stomach, strengthens the Spleen and Stomach and supplements qi
- Sp.6 (sanyinjiao +) strengthens the Spleen and supplements qi
- Bl.62 (shenmai), SI.3 (houxi); master and couple points of yangqiaomai, can assist in elevating qi to the upper body
- with spontaneous sweating, add LI.4 (hegu) and Kid.7 (fuliu)
- with thin, watery sputum, add St.40 (fenglong -) and Sp.3 (taibai +)
- with palpitations or bradycardia, add Ht.5 (tongli +)
- Ear points: lung, heart, spleen, zero point, shemen, sympathetic
Clinical notes
Fainting and blackouts associated with collapsing da qi may be a serious condition associated with cardiac weakness or failure, cardiopulmonary disease, cor pulmonale, emphysema, atrial fibrillation, ventricular tachycardia or sick sinus syndrome. Light exercise, especially swimming and easy walking, are recommended.
Qi and Blood Deficiency
Fainting and turns associated with qi and blood deficiency are common. Fainting and turns may occur because there is not enough qi and blood to maintain adequate pressure in the head when changing position. Fainting may also occur because the supply of qi and blood to the Heart is insufficient, and any extra load on the Heart causes arrhythmia and a sudden drop in circulation.
Clinical features
- Sudden fainting or transitory disturbance of consciousness, usually upon rising from a recumbent position. Episodes are associated with palpitations, spots or blurring in the visual field, weakness or loss of vision. The patient usually recovers quickly.
- dry skin and hair, pale complexion, nails and conjunctivae
- palpitations, arrhythmia, tachycardia brought on by exertion
- insomnia, dream disturbed sleep
- forgetfulness, poor memory, poor concentration
- spontaneous sweating and/or night sweats
- fatigue and weakness, breathlessness
- dry stools or constipation
- T: pale and maybe swollen with a thin coat
- P: thready and weak, or irregular
Treatment principle
Strengthen the Spleen and supplement qi and blood
Variations
Heart qi deficiency with arrhythmia
Heart qi deficiency causes fainting associated with sudden arrhythmia or ventricular tachycardia. Depending on the degree of deficiency, arrhythmias of a qi deficiency type can be sporadic and difficult to detect, occurring only when the patient is tired or suffering periods of stress. In such cases the arrhythmia may only be evident prior to fainting. When fainting is frequent however, the degree of deficiency is usually more profound, and irregularities will be noted on the pulse. The more irregular the heartbeat the greater the deficiency. The treatment is to supplement qi and blood, unblock yang qi and restore the pulse.
With chronic bleeding
Chronic bleeding can lead to significant qi and blood deficiency. It may go undetected, especially when occurring in the upper digestive tract. The bleeding may only be detected by a stool test. Bleeding of a qi deficiency type may also be seen in easy bruising or heavy periods. The treatment is to supplement Heart blood and Spleen qi, and stop bleeding.
Acupuncture (select from)
- Du.20 (baihui +∆) elevates yang qi and blood to the head
- Ren.12 (zhongwan +∆) alarm point of Stomach, strengthens the Spleen and Stomach and supplements qi and blood
- St.36 (zusanli +∆) sea point of the Stomach, strengthens the Spleen and Stomach and supplements qi and blood
- Sp.6 (sanyinjiao +∆) strengthens the Spleen and Kidneys, and supplements qi and blood
- Bl.20 (pishu +∆) transport point of the Spleen, strengthens the Spleen and supplements qi and blood
- Ren.4 (guanyuan +∆) supplements yuan qi
- Ren.6 (qihai +∆) boosts the Kidneys and regulates qi
- with bruising, heavy periods or occult bleeding, add Sp.1 (yinbai ∆)
- with sweating, add Ht.6 (yinxi +)
- with arrhythmia, add Ht. 5 (tongli) and Bl.15 (xinshu +)
- with insomnia, add Ht.7 (shenmen +) and anmian (N-HN-54)
- Ear points: heart, spleen, shenmen, sympathetic, adrenal
Clinical notes
Fainting and funny turns of a qi and blood deficiency type may be diagnosed as anemia, pregnancy, postural hypotension, hypoglycemia, cardiac arrhythmias, Stokes-Adams attacks or mitral valve prolapse. Qi and blood deficiency generally responds well to treatment, in combination with an appropriate supplementing diet. Treatment should be sustained for several months for a satisfactory result.
Heart Qi and Yin Deficiency
Fainting from Heart qi and yin deficiency can be caused by damage to fluids and qi by a prolonged or serious febrile illness, dehydration caused by vomiting, diarrhea or inadequate fluid intake. Heart qi and yin can also be depleted by chronic use of heating, dispersing or stimulant drugs such as amphetamines, cocaine, antihypertensives and steroids. The weakened circulation of qi and blood that is characteristic of heart qi deficiency is compounded by lack of yin fluids and increased viscosity of blood. This pattern is often complicated by blood stasis.
Clinical features
- Fainting, drop attacks or transitory disturbances of consciousness preceded by dizziness, light-headedness, flushing and hyperventilation
- palpitations, tachycardia, bradycardia, breathlessness
- spontaneous sweating and/or night sweats
- dry mouth and throat, dry stools, or constipation
- fatigue, lethargy and weakness
- anxiety, insomnia
- T: reddish, swollen and dry with little or no coat, or with multiple surface cracks
- P: thready, weak, or intermittent or irregular
Treatment Principle
Supplement Heart qi and yin
Strengthen the Heart and restore the pulse
Acupuncture (select from)
- Ht.7 (shenmen +) source point of the Heart, calms the shen, regulates and supplements Heart qi
- Ren.4 (guanyuan +) supplements yuan qi
- St.36 (zusanli +) sea point of the Stomach, strengthens the Spleen and Stomach and supplements qi
- Sp.6 (sanyinjiao +) strengthens the Spleen and Kidneys, nourishes qi and yin
- Ren.17 (shanzhong) regulates qi in the chest
- Bl.15 (xinshu +) transport point of the Heart, supplements Heart qi and yin, calms the Heart and Shen
- Bl.23 (shenshu +) transport point of the Kidney, supplements source qi and yin and supports the qi and yin of the whole body
- yintang (M-HN-3) calms the shen
- with arrhythmia, add Ht.5 (tongli +)
- with spontaneous sweating, add Bl.43 (gaohuangshu) and Du.14 (dazhui ∆)
- with night sweats, add Ht.6 (yinxi) and Kid.7 (fuliu)
- with chest oppression, add PC.6 (neiguan -)
- Ear points: heart, shenmen, spleen, stomach, sympathetic
Clinical notes
Fainting and turns of Heart qi and yin deficiency type may be associated with hypotension, atrial fibrillation, arrhythmias and sick sinus syndrome. Mild aerobic exercise is important to help rebuild qi and yin. Especially good are taijiquan, qigong and yoga. A review of the patient’s medications may be warranted. Illicit stimulant drugs should be strictly prohibited.
Heart Yang Deficiency
Heart yang deficiency causes fainting and turns because Heart function is seriously compromised. The Heart is too weak to adequately propel blood to the head, and the Heart is liable to sudden arrhythmia, further weakening the already poor circulation. Heart yang deficiency is frequently complicated by Kidney yang deficiency, blood stasis and/or phlegm.
Clinical features
Frequent fainting or drop attacks
- pale or ashen complexion; purple lips
- chest oppression, chest pain
- bradycardia, arrhythmia, palpitations
- breathlessness; in severe cases dyspnea or orthopnea
- spontaneous sweating, fatigue, weakness, exhaustion
- icy cold extremities, blue or purple discolouration of the extremities
- edema of the lower limbs
- all symptoms aggravated by exertion
- with blood stasis: stabbing chest pain, angina, purple or mauve tongue with dark distended sublingual veins
- with phlegm: marked chest oppression, thick tongue coat
- T: pale, swollen and scalloped
- P: deep, weak or imperceptible, or shallow and irregular or irregularly irregular
Treatment principle
Warm and supplement Heart yang
Variations
Kidney yang deficiency
Once Heart yang is responding to treatment and getting stronger, a more supplementing approach can be phased in. The aim is to strengthen the source yang qi, the Kidneys and thereby support the Heart. The treatment is to warm and supplement Kidney and Heart yang.
Acupuncture (select from)
- Bl.15 (xinshu +∆) transport point of the Heart, warms and activates circulation of Heart yang
- Bl.25 (shenshu +∆) transport point of the Kidneys, warms Kidney yang to support Heart yang
- Du.4 (mingmen +∆) warms and supplements Kidney yang to support yang systemically
- Ren.17 (shanzhong) improves circulation of yang qi through the chest
- PC.6 (neiguan -) connecting point of the Pericardium, opens up the flow of yang qi through the chest
- Ren.4 (guanyuan +∆) warms Kidney yang to support Heart yang
- St.36 (zusanli +∆) sea point of the Stomach, strengthens the Spleen and Stomach and supplements yang qi
- with arrhythmia, add Ht.7 (shenmen +) and Ht.5 (tongli)
- with chest pain, add PC.4 (ximen -)
- with blood stasis, add Bl.17 (geshu) and Bl.18 (ganshu)
- with sweating, add Du.14 (dazhui ∆)
- with edema or watery cough, add Ren 9 (shuifen ∆) and St.28 (shuidao ∆)
- for emergency management of collapsing Heart yang, see Box 4 in Part 1 of this article.
- Ear points: heart, kidneys, shenmen, adrenal, sympathetic
Clinical notes
Fainting of a Heart yang deficiency type may be associated with cardiac arrhythmia, atherosclerosis, arteriosclerosis, cardiomyopathy, congestive cardiac failure, sick sinus syndrome, mitral valve prolapse or Stokes-Adams attacks. Exercise is difficult for patients with yang deficiency, but can be helpful when undertaken in a controlled fashion. Gentle physiotherapy in a warm pool is a good way to begin.
Liver Qi Constraint with Blood Deficiency
Liver qi constraint with blood deficiency is more likely to causes funny turns than fainting. There are two mechanisms at play. The pent-up qi can suddenly be released and counter-flow to the head. The blood deficiency compounds the likelihood of developing qi constraint, can fail to rise to the head and not anchor the hun. The more blood deficiency, the more the likelihood of fainting. There is a clear stress component to this pattern but, paradoxically, turns or fainting of this type often occur sometime (weeks to a couple of months) after the stress has subsided. Patients are often able to “soldier on” through a difficult time, but as soon as they relax, the effects of the qi constraint on the body become apparent and turns occur.
Qi constraint is a precursor to other pathology implicated in fainting and funny turns. Prolonged qi constraint can slow and congeal fluids into phlegm, slow and stagnate blood, and generate heat and fire which damage yin and lead to ascendant yang or wind.
Clinical features
- Turns with sudden loss of balance, giddiness, blurring vision, disturbed proprioception and spatial disorientation, or rarely fainting. Restoration of normal consciousness is usually quick. Turns can be preceded by sudden rotation of the head, stress or emotional upset, or occur around the menstrual period.• postural dizziness, light-headedness
- fatigue, lethargy, worse in the morning and with inactivity
- irritability, depression
- muscular stiffness and tightness in the upper back and neck
- tension headaches; occipital and temporal headaches
- shallow breathing; tightness in the chest; frequent sighing
- sleep disturbance; typically waking between 1-3am
- constipation and sluggish stools, or alternating constipation and diarrhea
- heartburn, reflux, belching, abdominal bloating, loss of appetite
- T: normal color or mauve, or with pale or orangey edges and a thin coat
- P: wiry and thread
Treatment principle
Dredge the Liver and relieve qi constraint
Strengthen the Spleen and supplement qi and blood
Acupuncture (select from)
- Du.20 (baihui), GB.20 (fengchi -) these points regulate qi, subdue ascendant yang qi and clear the mind
- Ren.12 (zhongwan -) alarm point of the Stomach, strengthens the Spleen and supplements qi
- PC.6 (neiguan -) regulates Liver qi, downbears counterflow qi
- GB.34 (yanglingquan -) regulates the Liver and subdues ascendant yang qi
- Sp.6 (sanyinjiao +) strengthens the Spleen and supplements blood, dredges the Liver
- Liv.3 (taichong -) source point of the Liver, regulates Liver qi and blood, and nourishes Liver blood
- Bl.18 (ganshu -) transport point of the Liver, mobilizes Liver qi and activates blood
- Bl.20 (pishu +) transport point of the Spleen, supplements qi and bloodahshi points - tender points on the upper back and neck (sternocleidomastoid, trapezius)
- with Spleen deficiency, add St.36 (zusanli +)
- with tight neck and shoulders, add (GB.21 (jianjing -)
- with blurring vision, add GB.37 (guanming)
- with marked dizziness, add GB.43 (xiaxi -)
- with insomnia, add SJ.5 (waiguan) and GB.39 (xuanzhong)
- Ear points: shenmen, liver, zero point, sympathetic
Clinical notes
Fainting of a Liver qi constraint type may be diagnosed as an autonomic nervous system imbalance, vasovagal syncope, anemia or transient ischemic attack. Trigger points in the sternocleidomastoid muscle are a common contributor to dizziness and turns, and are commonly found in patients with Liver pathology. The posterior neck muscles and trapezius should also be assessed for tightness and trigger point activity, and treated if necessary. Exercise is an important component of treatment along with dietary modification. Hot spot therapy can also be helpful. (See article on Hot spot therapy on next page)
Ascendant Liver Yang, Liver Fire
Ascendant Liver yang is a severe form of counterflow Liver qi. Ascendant Liver yang or Liver fire are seen in younger patients without significant deficiency. As the patient ages or the condition persists, yin deficiency usually starts to intervene and the ascendant yang becomes more severe. In patients over 40, it is unusual to see ascendant yang without some underlying deficiency. In practice, the distinction between pent up Liver qi, ascendant Liver yang or fire and Liver yin deficiency with ascendant yang is rarely clear cut. Many patients will have elements of all patterns.
In this pattern, Liver yang ascends rapidly when severely constrained qi is suddenly released. Fire rises because it is its nature to do so. Fire is hotter and drier and may cause hemorrhages. Liver fire is more likely to develop if there is existing internal heat or a heating diet.
Clinical features
- Fainting, disturbances of proprioception and spacial orientation, vertigo, sense of heat rushing to the head or heat in the chest, visual disturbances or loss of balance initiated or aggravated by stress, anger or emotional upset, alcohol consumption, or sudden rotation of the head. The episode may be preceded or followed by migraine, fullness and distension in the head and eyes and nausea and vomiting.
- tension or migraine headaches; distending sensation in the head
- blurring vision, red, sore, gritty eyes
- irritability, short temper, anger outbursts, easily ‘flies off the handle’, red complexion or facial flushing
- right sided hypochondriac pain
- insomnia, dream disturbed sleep; waking between 1-3 am
- muscle spasms and tics
- T: red, or with red edges and a yellow coat
- P: wiry, strong and rapid
Treatment principle
Calm the Liver and subdue ascendant yang
Clear heat and fire
Acupuncture (select from)
- Du.20 (baihui -), St.8 (touwei); these points subdue ascendant Liver yang
- GB.20 (fengchi -) calms the Liver and subdues ascendant yang
- Liv.3 (taichong -) source point of the Liver, activates Liver qi, subdues Liver yang, extinguishes wind and alleviates spasms
- GB.34 (yanglingquan -) soothes the Liver and subdues yang
- GB.43 (xiaxi -) clears heat and subdues yang
- Bl.18 (ganshu) transport point of the Liver, moves Liver qi
- Bl.23 (shenshu +) transport point of the Kidney, nourishes Kidney yin to restrain and anchor yangahshi points - tender points on the upper back and neck (sternocleidomastoid, trapezius)
- with Liver fire, add Liv.2 (xingjian -)
- with muscle spasm in the neck, add GB.21 (jianjing -) and Du.9 (zhiyang -)
- with blurring vision, add GB.37 (guanming)
- with anxiety or headache, add yintang (M-HN-3)
- with insomnia and headache, add SJ.5 (waiguan -) and GB.39 (xuanzhong -)
- with nausea, add PC.6 (neiguan -)
- Ear point: liver, kidney, ear apex ↓, lowering blood pressure groove ↓The fainting and turns associated with ascendant Liver yang or fire may be diagnosed as transitory ischemic attacks, migraine or cluster headaches, an impending stroke, hypertension, eclampsia, puerperal fever or Meniere’s disease. Fainting or turns of an ascendant yang or fire type may represent a potentially dangerous condition or an impending catastrophe. Trigger points in the sternocleidomastoid muscle are a common contributor to dizziness and problems with proprioception, and are commonly found in patients with Liver pathology. The posterior neck muscles and trapezius should also be assessed for tightness and trigger point activity, and treated if necessary. Hot spot therapy in the region of T7-T10 can be helpful. A cooling diet can be helpful and regular exercise and stress management are essential components of successful long term treatment.
Liver and Kidney Yin Deficiency with Ascendant Yang or Wind
Liver and Kidney yin deficiency with ascendant yang is a mixture of deficiency and excess, and depending on their balance, the nature and intensity of symptoms carries. The pattern can oscillate between the background yin deficiency and the sudden manifestation of the ascendant yang. Patients have periods when the yang is more unanchored, fainting and turns are frequent, and active steps to subdue it are required. When the yang is more stable, the focus of treatment shifts to rebuilding the yin.
Liver yang rises because the yin is unable to anchor it and provide a counterweight to its active and rising nature. The yang loses its mooring and becomes excessively mobile, rising suddenly to the head. When ascendant yang reaches a certain level of intensity, it may be redefined as wind. The instability of the unanchored yang here is such that minor triggers are sufficient to cause it to ascend. Liver and Kidney yin deficiency with ascendant yang is often complicated by phlegm, phlegm heat or blood stasis.
Clinical features
- Fainting or drop attacks, or frequent disturbances of proprioception and spacial orientation, dizziness and vertigo, sense of heat rushing to the head, visual disturbances or loss of balance. Symptoms can be initiated or aggravated by stress, or emotional upset, sexual activity or sudden rotation of the head. The episode may be preceded or followed by migraine, distension in the head and eyes, and nausea and vomiting.
- tics, tremors, muscle spasms and fasciculation; numbness in the extremities
- blurred vision or visual disturbances, pressure behind the eyes
- temporal or vertex headaches; distending sensation in the head insomnia or restless sleep with much dreaming
- palpitations, anxiety, irritability and restlessness• red complexion, facial flushing or malar flushing
- sensation of heat in the chest, palms and soles; night sweats
- weakness, fatigue, exhaustion
- lower back ache and weakness; tinnitus
- T: red and dry with little or no coat
- P: wiry, thready and rapid
Treatment principle
Subdue and anchor Liver yang and extinguish wind
Nourish and supplement Liver and Kidney yin to anchor yang
Acupuncture (select from)
- Du.20 (baihui -), St.8 (touwei); these points subdue ascendant Liver yang
- GB.20 (fengchi -) calms the Liver and subdues ascendant yang
- Bl.18 (ganshu +), Bl.23 (shenshu +) transport points of the Liver and Kidney, nourish Liver and Kidney yin to secure and anchor yang
- Ren.4 (guanyuan +) supplements Kidney yin to anchor yang
- Kid.3 (taixi +) source point of the Kidneys, supplements Kidney yin and clears heat from deficiency
- Kid.6 (zhaohai +) supplements Kidney yin and clears heat from deficiency
- GB.34 (yanglingquan -) dredges the Liver and subdues yang
- Liv.3 (taichong -) source point of the Liver, subdues ascendant yang, extinguishes wind and alleviates spasms.
- ahshi points - tender points on the upper back and neck (sternocleidomastoid, trapezius)
- with muscle spasm in the neck, add GB.21 (jianjing -) and Du.9 (zhiyang -)
- with blurring vision, add GB.37 (guanming)
- with anxiety or headache, add yintang (M-HN-3)
- with insomnia and headache, add SJ.5 (waiguan -) and GB.39 (xuanzhong -)
- with nausea, add PC (neiguan -)
- Ear points: liver, kidney, ear apex ↓, lowering blood pressure grove ↓
Clinical notes
The fainting and turns associated with yin deficiency and ascendant yang may be associated with transitory ischemic attacks, vertebrobasilar insufficiency, atherosclerosis, arteriosclerosis, hypertension, post-concussion syndrome or disorders of the cerebellum.
This pattern can respond well to treatment; however, persistent fainting or disturbances of consciousness requires thorough investigation. This can be a potentially dangerous situation indicating an impending stroke in some patients, so frequent monitoring of subjective and objective signs, including blood pressure is necessary. In many cases, patients will be taking some form of antihypertensive medication. Interactions between antihypertensives and the prescriptions recommended for treatment are uncommon. However, the additive effect on blood pressure can be significant and low blood pressure may result. Patients should be alerted to the signs of low blood pressure (postural dizziness being the main one) and referred to their physician for a review of medication.
Trigger points in the sternocleidomastoid muscle are a common contributor to dizziness and problems with proprioception, and are commonly found in patients with Liver pathology. The posterior neck muscles and trapezius should also be assessed for tightness and trigger point activity, and treated if necessary. Hot spot therapy in the region of T7-L2 can be helpful along with regular exercise, stress management and a yin nourishing diet.
Phlegm Damp Blocking the Channels of the Head and Muscles
Phlegm damp causes disturbances of consciousness and turns in two ways. It clogs up the channels and impedes the normal circulation of yang qi to the head and muscles, and it sits like a veil over the senses. Without adequate yang qi getting to the head and muscles, and with the senses clouded, the patient experiences mental dullness, somnolence or sudden loss of muscle function.Turns and disturbances of consciousness of a phlegm damp type can be intermittent, appearing in clusters for a period of time, after which the patient is comparatively normal until the episodes begin again. This sporadic course is due to the alternate congealing and dispersal of phlegm, which occurs in response to changes in diet or increases in emotional tension.
Clinical features
- Sudden loss of muscle function causing collapse without loss of consciousness. In mild cases there may only be limpness of the neck or knees, sagging facial muscles or inability to speak clearly. The collapse may be triggered by emotion. Episodes last from seconds to minutes, after witch normal function is restored.
- Irresistible sleepiness during the day, often worse in the afternoon and after eating. The patient may fall asleep without warning. After restoration of consciousness the patient may be quite groggy for a period of time.
- foggy head, difficulty concentrating; dizziness and vertigo
- heaviness and lethargy
- headaches, dull distension in the head
- fullness in the abdomen, chest oppression
- mucus congestion, throat clearing
- loss of appetite, loss of sense of taste, nausea, vomiting, belching, acid reflux, loose stools, or occasionally constipation (but stools are not dry)
- even though the condition is chronic, the patient appears robust and may be overweight
- T: thick, greasy, white coat, possible swollen or flabby body
- P: slippery or wiry or moderate
Treatment principle
Dry damp and transform phlegmStrengthen the Spleen and correct the qi dynamic
Acupuncture (select from)
- Du.20 (baihui -) clears phlegm from the head
- GB.20 (fengchi -) calms the Liver, clears the head and subdues yang
- PC.5 (jianshi -) river point of the Pericardium, transforms phlegm
- Sp.3 (taibai), St.40 (fenglong-); source and connecting point of the Spleen and Stomach to strengthen and transform phlegm damp
- Bl.62 (shenmai), K.6 (zhaohai); master points of dumai and yinqiaomai, used on alternate sides for inability to keep the eyes open
- St.41 (jiexi -) river and fire point of the Stomach, strengthens the Spleen and Stomach to transform phlegm damp
- St.36 (zusanli +∆) sea point of the Stomach, arms and strengthens the Spleen and Stomach, supplements yang qi
- Bl.20 (pishu) transport point of the Spleen, strengthens and supplements Spleen qi and yang to promote transformation of damp and phlegm.
- with Liver qi constraint, add GB.34 (yanglingquan -) and Liv.3 (taichong -)
- with cold, apply moxa cones to Bl.20 (pi shu) and BL.21 (weishu)
- with muscle aches, add Sp.21 (dabao)
- with abdominal distension, add St.25 (tianshu -) and Sp.15 (daheng)
- Ear points: spleen, sero point, liver, subcortex, sympathetic, shenmen, lowering blood pressure groove ↓
Clinical notes
Turns and disturbances of consciousness associated with phlegm damp may be diagnosed as narcolepsy, catalepsy, food allergies, hypoglycemia or chronic fatigue syndrome. This pattern can respond to treatment but depending on the duration of the condition and the age of the patient can take a long time to achieve a satisfactory result. The heaviness and lethargy typical of phlegm damp can be impediments to exercise, but graded exercise in groups can achieve good results. Diet is an important part of phlegm damp treatment. Avoidance of certain foods is important if there is intolerance or allergy. Hot spot therapy can also be helpful.
Wind Phlegm
Wind phlegm is a pattern that combines the sudden onset and involuntary movement of wind with the consciousness clouding phlegm. There are two types of consciousness disturbance associated with wind phlegm, depending on the balance of wind and phlegm. The first is associated with severe vertigo and spatial disorientation to the point of falling but without loss of consciousness and occurs when the phlegm component is greater than the wind. The second is associated with fainting, involuntary movement, spasms or convulsions, and is due to the dominance of the wind over the phlegm.
Phlegm causes consciousness disturbances by clogging the senses, like a “mist”. When fainting occurs, the phlegm is carried swiftly to the head by wind. This pattern is often complicated by Spleen qi deficiency and ascendant Liver yang.
Clinical features
- Phlegm dominant: Confusion, befuddlement, vertigo, disordered proprioception and spacial disorientation, or sudden collapse, usually preceded by vertigo and headaches. Episodes may be triggered by movement of the head, exposure to strong smells like perfume and gasoline or emotional upheaval. After the episode the patient is groggy, sick and disoriented for a period afterward.
- Wind dominant: abrupt impairment of consciousness and muscle twitching without collapse (‘absence’ seizure), loss of voluntary control over a limb or collapse and convulsions.
- dull headaches and head distention, tinnitus
- heaviness in the body, lethargy, fatigue
- nausea for vomiting; nausea may precede episodes
- abdominal distention, chest oppression
- T: swollen, with a thick, greasy, white coat
- P: slippery and wiry or soft and soggy
Treatment principle
Transform and disperse phlegm and extinguish wind
Strengthen the Spleen and Stomach and regulate qi
Acupuncture (select from)
- Du.20 (baihui -), St.8 (touwei); these points clear phlegm from the head
- GB.20 (fengchi -) clears the head, regulates qi and subdues yang
- Ren.12 (chongwan) alarm point of the Stomach, strengthens Stomach and Spleen function to transform phlegm
- Liv.13 (changmen -) alarm point of the Spleen and meeting point of the internal organs, strengthens the Spleen and improves digestion, promotes Liver function
- PC.5 (jianshi -) river point of the Pericardium, transforms phlegm
- GB.34 (yanglingquan -) subdues yang and windSp.3 (taibai +), St.40 (fenglong -) source and connecting points of the Spleen and Stomach, transform phlegm
- Sp.5 (shangqiu -) metal points of the Spleen, transforms damp, strengthens the Spleen
- St.41 (jiexi -) fire point of the Stomach, strengthens the Spleen and Stomach to transform phlegm
- with Spleen deficiency add St.36 (zusanli +)
- with Liver qi constraint, add GB.34 (yanglingquan -) and Liv.3 (taichong -)
- with foggy head, add Bl.62 (shenmai)
- with cold, apply moxa cones to Bl.20 (pishu ∆) and Bl.21 (weishu ∆)
- with muscle aches, add Sp.21 (dabao)
- with edema, add Sp.9 (yinlingquan -) and Sp.6 (sanyinjiao)
- with somnolence, add Kid.6 (zhaohai) and BL.62 (shenmai)
- Ear points: stomach, spleen, zero point, subcortex, sympathetic, shemen
Clinical notes
Fainting or turns of this type are likely to be diagnosed ad Meniere’s disease, labyrinthine disorders or epilepsy. Wind phlegm can respond reasonably well to persistent treatment and provide some symptom control. Diet is an important part of phlegm treatments.
Food Stagnation, Stomach Heat
Fainting from food stagnation is associated with overeating or ingestion of specific foods. As a result of overeating, qi is drawn away from the periphery and head, the qi dynamic and qi distribution are disrupted. Certain foods can trigger episodic fainting or turns in susceptible patients, in particular items such as aged cheese, fermented foods, chocolate, red wine and sulfites used as preservatives. The main treatment is to avoid overeating and the known food triggers, but in some chronic cases even small amounts of food can initiate an episode.
Clinical features
- Fainting after eating a large meal or specific foods. Episodes may be preceded by visual disturbances, facial flushing, breathing difficulty or food cravings. Recovery can be gradual and accompanied by pallor, nausea, vomiting, and throbbing headache.
- abdominal and epigastric distention or pain, relieved by belching or flatulence, constipation, difficult or irregular stools, or occasional diarrhea
- halitosis, acid reflux, heartburn, nausea or vomiting, copious foul flatulence
- T: thick, white or yellow, greasy coat
- P: wiry and slippery or slippery and rapid.
Treatment principle
Disperse accumulated food, resolve stagnation and clear heat
Acupuncture (select from)
- Ren.12 (zhongwan -) alarm point of the Stomach, clears heat and disperses food stagnation
- St.25 (tianshu -) alarm point of the Large Intestine, regulates Intestinal function
- Ren.6 (qihai -) regulates qi and alleviates distention
- St.36 (zusanli -) sea point of the Stomach, regulates and strengthens the Stomach and Intestines
- LI.10 (shousanli -) benefits digestion and regulates gastrointestinal function
- ST.44 (neiting -) water point of the Stomach, clears heat form the Stomach and Intestines and disperses stagnant food
- with constipation, add St.37 (shangjuxu -) and SJ.6 (zhigou -)
- with abdominal pain, add St.34 (liangqiu -) and Sp.4 (gongsun-)
- with nausea, add PC.6 (neiguan -)
- with Spleen deficiency, add sp.6 (sanyinjiao)
- with borborygmus, add Sp.5 (shangqiu -)
- Ear points: zero point, spleen, stomach, liver, abdomen
Clinical notes
Fainting associated with food stagnation may be diagnosed as allergy, gastroesophageal reflux or migrainous syncope. The main treatment is regulation of the diet and avoidance of known triggers. Even though the etiology is overeating or food allergy, it is the heat that has been generated that must be cleared, and this can take a while. Treatment should persist for at least two to three weeks, in conjunction with appropriate dietary modification.
Blood Stasis
Fainting and funny turns due to blood stasis may be acute or chronic. When acute, there will usually be a history of head trauma; when chronic, there is often a long history of constrained Liver and Heart qi. The presence of static blood obstructs the free movement of qi and blood in the network vessels and obstructs the distribution of yin and yang in the head and sensory orifices.
Clinical features
- Loss of balance, dizziness, disturbed proprioception and spatial disorientation, blurring vision, amnesia, or fainting
- purplish complexion, lips, sclera, conjunctiva and nail beds
- dark rings around the eyes
- palpitations, chest pain and/or persistent localized palpitations, bradycardia headaches
- insomnia, fitful sleep disturbed by low grad or hectic fever
- depression, mood swings• dry scaly skin
- broken vessels or spider nevi on the face, trunk, inner knee and ankle
- pressure pain in the left iliac fossa
- T: in acute cases following head trauma the tongue body may be unremarkable; in chronic cases it will be mauve or purple, or with brown or purple stasis spots and a thin, white coat; sublinigual veins are congested and dark
- P: deep, thready, choppy, wiry or intermittent
Treatment principle
- Activate qi and blood and dispel blood stasis
- Acupuncture (select from)
- Du.20 (baihui -) clears the head
- GB.20 (fengchi -) dispels and extinguishes wind, calms the Liver and subdues Liver yang, clears the mind.
- ahshi points - tender points on the head, upper back and neck
- SI.3 (houxi -), Bl.62 (shenmai); the master and couple points of dumai qi to assist in moving blood through the head
- Bl.17 (geshu -) meeting point for blood, transforms and dispels stagnant blood
- Sp.6 (sanyinjiao -), Sp.10 (xuehai -), Li.4 (hegu -); these points activate blood and dispel static blood
- Liv.3 (taichong -) source point of the Liver, dredges the Liver and activates the blood
- with trauma, add points of pain on the head (ahshi)
- with depression, add LI.4 (hegu) and Liv.3 (taichong)
- Ear points: head, brain, liver, heart, sympathetic, shenmen
Clinical notes
Fainting and turns of a blood stasis type may be diagnosed as the sequelae of concussion, tumors in the head, cerebellar lesions, cardiac arrhythmias, sick sinus syndrome, Stokes-Adams attacks, vertebrobasilar insufficiency, congestive cardiac failure or angina. A qi and blood mobilizing diet is appropriate.
Hot Spot Therapy
 Hot spot therapy is a technique that utilizes sustained pressure on specific points along the Urinary Bladder channel. The technique is based on the external manifestation, through the channel pathway and associated tissues, of internal organs system dysfunction. When a particular organ system is in a pathological state the paraspinal muscles of the affected segment are usually tight or knotted. The muscle tightness constricts the vessels and nerves passing through it and further impedes the flow of qi and blood. Releasing some of this tension has a beneficial effect on qi and blood movement through the segment, and on the function of the underlying organ system.
Hot spot therapy is a technique that utilizes sustained pressure on specific points along the Urinary Bladder channel. The technique is based on the external manifestation, through the channel pathway and associated tissues, of internal organs system dysfunction. When a particular organ system is in a pathological state the paraspinal muscles of the affected segment are usually tight or knotted. The muscle tightness constricts the vessels and nerves passing through it and further impedes the flow of qi and blood. Releasing some of this tension has a beneficial effect on qi and blood movement through the segment, and on the function of the underlying organ system.
The technique is quite simple; its success relies on regularity and persistence of application. In essence it is simply sustained pressure applied to specific loci, done by the patient at home for 10 minutes or so every day. The regular pressure on the appropriate spots gradually leads to a sustained softening of the superficial tissues, better qi and blood flow and improved organ function. The technique can be applied along the length of the erector spinae muscles, from Bl. 13 (feishu) to Bl.25 (dachangshu), with the main areas of interest usually the mid back, from Bl. 15 (sinshu) to Bl. 20 (pishu).
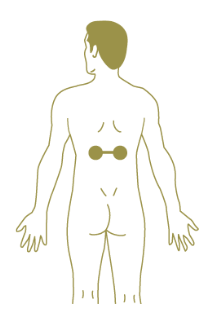
The technique involves a device made from two tennis balls placed in a sock with a knot tied between them. This enables the patient to apply pressure bilaterally with a ball sitting on both left and right Urinary Bladder channels with the knot over the spine (Fig.1). The patient lies on the bed or the floor with tennis balls placed on either side of the spine on the Urinary Bladder channel. Using their legs to move and make fine positional adjustments they seek the sorest sports, those with the most stagnation, and once located relax into them and let their body weight provide the required pressure. The pressure should be strong and may initially hurt, but should not be so strong that the patient tenses up against it. If the pressure form the body weight is too much, a softer surface may help, in fact it is a good idea to always begin the technique on a bed and graduate to a harder surface as the stagnation resolves and firmer pressure is desired.
Once the points have been located and the pressure applied, it should be maintained for a few minutes, or until the soreness clearly decreases, the tension release and the points ‘give’. Once the ‘give’ has occurred, move on to another point. Two or three points should be treated and deactivated each session. Little by little the sore points should soften and relax. For those unable to lie, the technique can also be done in a firm chair or leaning against the wall. The time is important because what is being stimulated is a neurological reflex- the pressure sends a signal to the brain, which after a certain period, usually no longer than 90-120 seconds, sends a signal back to the muscle to release, the ‘give’. Pressure maintained after the release is unnecessary.
Tennis balls are selected because they have the right balance of firmness and elasticity to provide a good degree of pressure without undue discomfort. The technique is like having an acupressure massage every day. The benefits accumulate gradually, with persistent practice providing significant and sustained result. This technique is most useful in excess patterns, especially those with a component of Liver qi constraint.


