Laughter is Good Medicine
One brisk afternoon in the remote village of Kogate in the Southern district of Makawanpur, Nepal, several men and women bundled in many layers of brightly colored wool clothing, sat in the sun waiting for their turn to see the “Doctor.” Many of them had never seen a medical provider in their entire lives. Now, in their small village, our team of practitioners moved their chairs out into the small courtyard in front of the rustic clinic building, as it was too cold to treat indoors.
Some of the villagers waited many hours for their turn to tell the doctor about their pain, injury, or other health concern. Around the low stone wall that surrounds the courtyard, a dozen children and adults watched their friends and neighbors being treated. How strange this must have looked as our practitioners inserted several small needles into their patient’s bodies. A constant chatter filled the air as the villagers discussed the scene and asked their friends if the needles hurt. “Dhukdaina” they replied “It doesn’t hurt.”
 Sometime in the midafternoon a small boy of about 8 years was ushered into the clinic with a gaping head wound. Blood poured from a two inch gash and his skull was clearly visible in the opening. The practitioners quickly assessed the boy for a concussion and interviewed the clearly shaken mother about the cause of the injury. It was determined that the family did not have the resources to transport the boy to the regional hospital, which was nearly 3 hours away by a very expensive, fourwheel drive, ambulance ride.
Sometime in the midafternoon a small boy of about 8 years was ushered into the clinic with a gaping head wound. Blood poured from a two inch gash and his skull was clearly visible in the opening. The practitioners quickly assessed the boy for a concussion and interviewed the clearly shaken mother about the cause of the injury. It was determined that the family did not have the resources to transport the boy to the regional hospital, which was nearly 3 hours away by a very expensive, fourwheel drive, ambulance ride.
The team advised the mother about what they could do and what care would be required in the following days. They then proceeded to carefully clean the wound. A topical anesthetic (Lydocaine) was applied to help numb the area as damaged skin was clipped away with a scalpel and scissors. Finally the wound was closed with a medicalgrade super glue and suturing tape.
The boy was given a mild dose of Tylenol to help with the pain and some herbal antibiotic (clear toxic heat) tablets to help reduce the chance of infection. The mother was given a cup of tea while the practitioners did their work.
After the procedure was finished the team educated the mother on how to look for signs of a concussion or infection. She agreed to bring the boy back the following day (even though it was a several hour walk to the clinic) or sooner if the boy took a turn for the worse. They agreed upon a contingency plan to administer Dicloxacillin (an antibiotic drug) if the boy exhibited a fever or other signs of an infection.
This kind of visit to our clinic is not at all unusual but may seem atypical for an “Acupuncture Clinic.” In fact, much of our clinical practice does not involve acupuncture at all. Our teams regularly assist with child birth, respond to midnight emergencies, diagnose cases of cancer, parasitic infection and diabetes, and report suspected cases of polio to the World Healthcare Organization. We see our clinic as a new model in the delivery of primary healthcare in rural and developing regions.
In this model we utilize what we call the “best care available” rule in our treatment planning. We pride ourselves on our expert diagnostic and evaluation skills which help us determine our plan. We start by asking ourselves: What is the best care for this condition? Is that care available to this patient, and how do we help our patient’s access that care?
 Many times we conclude that acupuncture is the “best care” available because of its effectiveness in treating many conditions, especially pain and other inflammatory pathologies. Acupuncture is also very inexpensive, has very few side effects, and is easy to teach to other healthcare workers. Chinese herbal medicine, local Ayurvedic herbs, and naturopathic supplementation are also employed wherever they are deemed effective and they are very effective when used properly. In addition, we are authorized and provided 40 listed allopathic drugs by the District Health Office. We use this pharmacology sparingly and wisely.
Many times we conclude that acupuncture is the “best care” available because of its effectiveness in treating many conditions, especially pain and other inflammatory pathologies. Acupuncture is also very inexpensive, has very few side effects, and is easy to teach to other healthcare workers. Chinese herbal medicine, local Ayurvedic herbs, and naturopathic supplementation are also employed wherever they are deemed effective and they are very effective when used properly. In addition, we are authorized and provided 40 listed allopathic drugs by the District Health Office. We use this pharmacology sparingly and wisely.
For some of our patients, who have the means to travel to a regional heath post, we order labs and imaging (x-rays, ultrasounds, MRIs and CT scans). Many times we refer patients to specialists (surgeons, neurologists, gynecologist, etc). We partner with the local government and attempt to guide patient care through accurate reporting, good referral procedures and followup.
 Educating patients and healthcare workers is sometimes more important than all of our treatment modalities combined. Soap, water, and general hygiene become one of the most effective antibiotic treatments.
Educating patients and healthcare workers is sometimes more important than all of our treatment modalities combined. Soap, water, and general hygiene become one of the most effective antibiotic treatments.
In Nepal, pharmaceutical antibiotics are commonly overprescribed. This results in resistant strains of bacteria, allergic reactions and a general weakening of the patient’s digestive system. There is no counting the number of patients we have seen with damaged hearing due to uncontrolled chronic ear infections. Many of these patients have been given Amoxicillin irregularly for 10 or more years. The result is very hard to kill infections and irreparable damage to the tympanic membrane and middle ear structures. This affects many young people in Nepal and is completely preventable with better training and patient management.
This year, the Acupuncture Relief Project undertook the courageous challenge of opening three experimental clinics in the remote regions of Bhimphedi, Kogate and Ipa, all villages in the District of Makawanpur. For the first time since we began working in Nepal (2008), we achieved a full partnership with the local government. Operating under the Nepal Social Welfare Council in cooperation with the Makawanpur District Health Office, we are now subject to the necessary oversight, inspection and reporting requirements of other governmental and private healthcare institutions. While this adds some level of expense, bureaucracy and complexity to our operation, it also allows us a new level of authority and access to government assets such as facilities and medications.
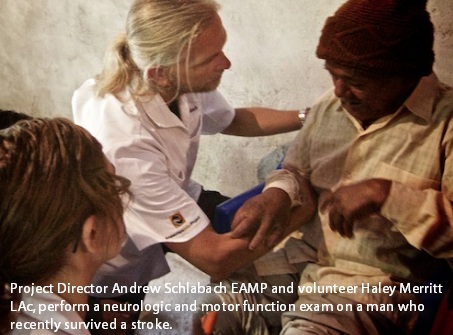
 In our first three months here, we provided over 7,000 primary care visits. Our volunteer practitioners work 6 days per week and tackle some of the most difficult medical cases found in any modern hospital. Tuberculosis, diabetes, stroke, domestic violence, alcohol abuse and seizures are common to our treatment rooms. Many times the “best care available” is the “only care available”... and that would be us.
In our first three months here, we provided over 7,000 primary care visits. Our volunteer practitioners work 6 days per week and tackle some of the most difficult medical cases found in any modern hospital. Tuberculosis, diabetes, stroke, domestic violence, alcohol abuse and seizures are common to our treatment rooms. Many times the “best care available” is the “only care available”... and that would be us.
Since we were attempting to operate in a new region, it was necessary to select and train several new language interpreters. We began by advertising for English speaking locals three months before opening our new clinic. We interviewed many and finally invited 15 students for training.
There is so much more to being an effective medical interpreter than just speaking English so we looked for students who not only possessed good language skills but also demonstrated empathy, sensitivity and a profound interest in their communities.
 At the end of our initial three week training session, we offered employment to eight. Our new crew of interpreters, aged 18 to 24, had never met a foreigner or spoken to a native English speaker. What they lacked in confidence, they made up for with determination.
At the end of our initial three week training session, we offered employment to eight. Our new crew of interpreters, aged 18 to 24, had never met a foreigner or spoken to a native English speaker. What they lacked in confidence, they made up for with determination.
Each week on their day off they attended classes taught by our volunteers. Classes included medical terminology, anatomy and physiology, safe clinical procedures, Chinese medical theory, concepts of therapeutic relationships, diet, and exercise. They also learned some basic auricular acupuncture protocols and massage techniques. All of this helped them become better at advocating for the information that practitioners needed to make a proper assessment.
Our interpreters are crucial to our success in the clinic. When starting in a new village, it is imperative that we gain the trust of the community and the skill of our interpreters enables us to make that critical personal connection to each of our patients.
This is no easy task. Our practitioners and interpreters work side-by-side all day, every day, slowly perfecting each other’s rhythm, emotion and syntax until they seamlessly work as one. Once this happens, it is a magical experience for both the patient and practitioner, and people start to get better.
 One of the things I find the most interesting in working with the interpreters is that they maintain a truly unique perspective on what it is that we do here. They are not familiar with our medicine... or any medicine for that matter. They are interested in what we do but they are more interested in what they are doing for the people of their communities.
One of the things I find the most interesting in working with the interpreters is that they maintain a truly unique perspective on what it is that we do here. They are not familiar with our medicine... or any medicine for that matter. They are interested in what we do but they are more interested in what they are doing for the people of their communities.
At a recent training meeting, I tasked our interpreters to list 10 ways they thought our clinic was helping the people of their village. I think every healthcare professional should take note: only one of their answers had anything to do with acupuncture or medicine at all.
Their number one answer was... “laughter is good medicine.” When I asked them to explain this, they elaborated that no one in Nepal had ever experienced a doctor that laughed with them, or took the time to know anything about their life outside of their health complaint let alone explain a diagnosis, treatment plan or medication.
The fact that everyone was treated exactly the same, with kindness and patience, regardless of their ethnic group, caste or socioeconomic status, was what our interpreters saw as our greatest contribution. They also commented that selfcare, proper use of medication and dietary advice we offer empowers people to take better care of their own health. Can it really be that simple?
As this project strives to integrate so many modalities and medical concepts into a model of accessible, effective and ethical care, I am struck by the notion that there is really no such thing as alternative medicine. When people work together because they truly care about the wellbeing of others... this is medicine.
Bio: Andrew Schlabach MAcOM EAMP is the co- founder and President of the Acupuncture Relief Project (ARP), a free primary care clinic utilizing acupuncture and integrative medicine in rural Nepal. Since inception in 2008, ARP teams have provided over 150,000 primary care visits and have offered an unparalleled training opportunity for their interpreting staff and volunteers alike. In 2013, ARP undertook a pilot program, opening three new clinic sites in the very remote region of Kogate, Nepal. Acupuncture Relief Project was also the subject of the short documentary entitled Compassion Connects: Ancient Medicine for Modern Health Care (2012), which you can watch in its entirely at their website www. acupuncturereliefproject.org
Schlabach practices in Vancouver, Washington at Healthwerks Acupuncture Wellness Clinic. He authored and published the Acupuncture and Chinese Herbal Medicine - Clinic Survival Guide , designed as an easy-to-use clinic reference of essential information for practitioners and students. While he was a master’s student at Oregon College of Oriental Medicine (OCOM), he was part of the group research project that created QIPARTNER, a practice-based research network for Oriental medicine practitioners and researchers in Oregon and Southwest Washington in collaboration with the Helfgott Research Institute.
Prior to his study of Oriental medicine, Schlabach served as President and Creative Director of Split Diamond Media, Inc. of Portland, Oregon for 15 years. As a veteran of the U.S. Army, he received an Army Commendation Medal for distinguished service to his unit. He is an accomplished mountaineer, gaining much expedition experience as an instructor at the Himalayan Mountain Institute in Darjeeling India.

